Colorectal cancer is the kind that begins in the colon or rectum. These cancers are also called colon cancer or rectal cancer, depending on where the cancer starts. Although many colorectal cancers can be prevented with regular colonoscopy screenings, it remains the third leading cause of cancer deaths in the U.S. among the general population.1
The average lifetime risk for colorectal cancer is approximately 5 percent, but for adults with cystic fibrosis, this risk is 5–10 times higher and warrants screening 5 years earlier, at 40 years of age.
Meanwhile, those who receive a solid organ transplant are 20 times more likely to develop colorectal cancer and often need to begin screening even earlier — age 30, depending on when the transplant occurs.
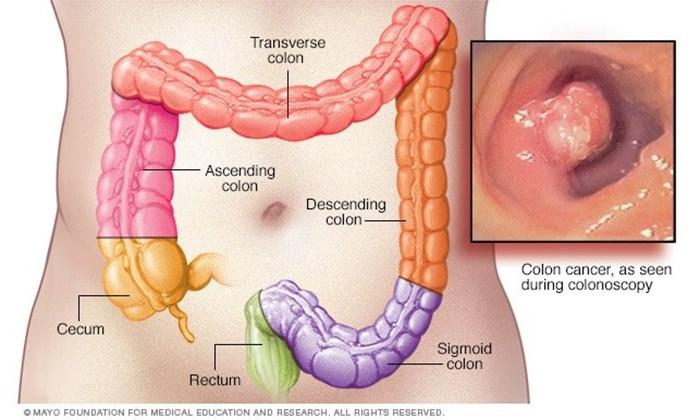
How Does Colorectal Cancer Form in the Body?
Most colorectal cancers start as a polyp — a small, abnormal growth of tissue that can develop on the inner lining of the colon or rectum. Most polyps are harmless (benign), but a certain kind of polyp, known as an adenoma, can become cancerous over time.
There are two general types of colon polyps:
- Hyperplastic polyps and inflammatory polyps: common polyps that do not generally develop into cancer.
- Adenomatous polyps: polyps that are considered pre-cancerous because they are more likely to develop into cancer.
It can take many years for a polyp to develop into cancer, but once the cancer forms, it can grow into the wall of the colon or rectum. When cancer cells are in the wall, they can then spread to surrounding tissues and, eventually, other parts of the body. The further the cancer spreads, the more difficult it is to treat.
Symptoms
In general, people with CF will experience many of the same symptoms of colorectal cancer as the general population, including:
- Blood in the stool.
- Abdominal pain that gets worse over time.
- Weight loss.
- Anemia.
- Abrupt changes in prior bowel habits (i.e., new or persistent constipation or diarrhea).
At the same time, however, many people report experiencing no symptoms before receiving a colorectal cancer diagnosis, which is why it is sometimes called the “silent cancer.” That is why screening is incredibly important.
Although the Cystic Fibrosis Foundation’s Colorectal Cancer Screening Clinical Care Guidelines recommend that people with CF begin screening at age 40, symptoms can be an indicator to begin screening even earlier. If you think you are experiencing colorectal cancer symptoms, talk to a member of your CF care team.
"Before I was diagnosed, I found blood in my stool one time and then, months later, had two days of stomachaches despite regularly taking my enzymes. At the time, however, I didn’t know about my increased risk for colorectal cancer and attributed it to CF-related digestion issues. I wish I had said something to my CF doctor about these small symptoms earlier when the cancer was still in its most curable stages." — Christine Borland, who had CF and colon cancer