When my newborn son, Ashton, first went to cystic fibrosis clinic 21 years ago, we spent three hours in a small room. There were no masks or infection prevention guidelines back then. We were not nearly as aware of infection risk as we have become. Fast forward to March 2020 and the fear of infection went into overdrive. I have two kids with CF -- Ashton and his 15-year-old sister Lola -- and COVID-19 was spreading through the West Coast. We were terrified, cleaning our groceries with disinfecting wipes and avoiding anyone outside of our home. How on earth could we be comfortable inside a hospital or CF clinic that had COVID-19 patients in the ICU?
After watching the first plenary of the North American Cystic Fibrosis Conference, “Meeting the Moment: Lessons Learned from a Changing World” from Michelle Prickett, MD, I realized how much work went on behind the scenes. Hours of Zoom meetings, data entry, rescheduling hundreds of appointments, and shifting responsibilities -- all while many CF team members cared for the sickest among us -- must have been exhausting and frustrating. I am filled with gratitude for the hoops that the CF clinic staff jumped through to make sure we continued to safely receive high-quality CF care during the pandemic.
Watch the full plenary on Facebook Live.
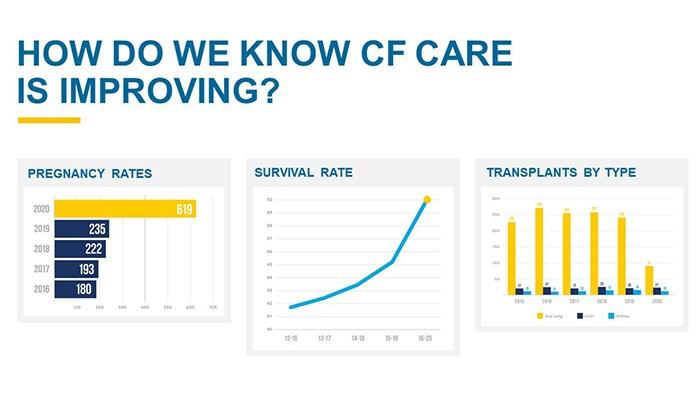
Many important measures improved last year, including an increased number of pregnancies, a jump in life expectancy, and fewer lung transplants.
If you had told me 20 years ago that the health of many people with CF would improve during a global pandemic caused by a deadly respiratory disease, I would have laughed at you while trying to get enzymes onto a spoonful of applesauce in a clinic exam room.
A few months before the lockdown, my children were lucky enough to start Trikafta®. Although Ashton did not experience amazing results because he also has a mitochondrial disease, Lola responded well. But, we didn't want to lose that momentum and positive benefits we attributed to the combination of Trikafta and personalized CF care from the clinic staff, and I worried that telehealth would negatively impact Lola's health. On the other hand, Ashton needed close monitoring of his lung function and other health issues. Would telehealth visits be enough to detect further decline in Ashton or any negative side effects in Lola? I didn't need to worry about it. With effective communication between my children and the clinic staff, occasional in-person visits, and the use of a home spirometer and scale, we successfully monitored my kids for any problematic issues.
Now in 2021, Ashton and Lola's CF clinic “visits” often means staying in pajamas, sitting at the kitchen table, and being a whole three feet away from the fridge for a snack. The result of the adaptation the CF clinic staff made means no traffic or parking hassles, no waiting rooms, no sick people sitting nearby. It is awesome! We love telehealth and believe it is a safe, convenient, effective tool that minimizes the time spent away from college, high school, and jobs and also allows for us to maintain positive relationships with all of the clinic staff.
We had to adapt, too. We needed to learn how to use a home spirometer so our care teams could monitor my kids' lung function and they could react to any changes that needed to be addressed. I turned to YouTube to learn how to do a throat culture for my son in the clinic parking lot so we could continue to track any potential infections while reducing COVID-19 exposure risk. Sadly, Ashton told me he prefers the experienced touch of our respiratory therapist …
As great as it can be, telehealth isn't necessarily the same positive experience for everybody as it is for my kids and me. And what about those patients who may not have access to the internet or the technology that is needed or those with more complicated cases who may decline without a hands-on approach?
As Dr. Prickett emphasized, equity in CF care must be addressed in access to telehealth, in modulator access, and equity in care for people with more severe cases of CF. Dr. Prickett also noted that as some people experience better health for a longer period of time, efforts must be made to bring everyone up to the same level of care need to begin now by focusing care resources on those who most need them.
Dr. Prickett addressed that CF care will continue to evolve and the thoughtful use of telehealth, the increased age of CF patients, and improvements in home monitoring may transform how and where my children will see their clinic team. There are so many possible benefits. My children might continue to see their current physicians when they move away for college or if they travel for long periods of time. Perhaps with continued advancements in CFTR modulators and other treatments, they will only need to see the team once or twice a year. It is a brave new world.
Dr. Prickett pointed out that CF is no longer a childhood disease. There are more adults with CF than children. CF care teams may need to expand in the future to include gerontologists, fertility specialists, and cardiologists. When my son was recovering from his traumatic start to life -- being born 11 weeks premature and needing a surgery to correct an intestinal blockage -- I never dreamed that either of my children could grow so old that they'd need a specialist to treat issues related to advanced age.
What will the next five years bring? Will the average life span hit 60? The future has arrived, and the CF community will be at the forefront of using the gift of telehealth, modulators, better access to new treatments, and the best clinical research of any foundation. Together, we will treat and beat CF better than anyone could have imagined.
Interested in sharing your story? The CF Community Blog wants to hear from you.