In the next five years, we expect between 90-95 percent of people with cystic fibrosis to benefit from highly effective treatments called cystic fibrosis transmembrane regulator (CFTR) modulators. These drugs correct the underlying cause of the disease by helping the defective protein function properly.
Unfortunately, about 5 percent of people with CF, because of their mutations, will never benefit solely from these medications as they do not produce any CFTR protein. Below, William Skach, M.D., senior vice president of research affairs at the Cystic Fibrosis Foundation, answers questions about the research the Foundation is funding to develop treatments for people with these types of mutations.
Q. Why is the Foundation focusing on research into mutations that prevent the production of CFTR proteins?
A. The CF Foundation is committed to ensuring that everyone with CF has an effective treatment that targets the underlying cause of their disease. We have made tremendous progress in the last few years, with CFTR modulators for nearly 60 percent of CF mutations, and we expect that number to grow significantly in the near future. However, about 5 percent of the CF population will not be able to benefit solely from modulators. That is why we are aggressively funding research to discover new treatments -- to ensure that no one is left behind and everyone benefits.
Q. Why can't this 5 percent of people benefit from CFTR modulators?
A. Every person with CF has two CFTR genes, each of which carries a mutation that decreases CFTR protein function, and, because different mutations cause different defects in the protein, CFTR modulators are only effective in people with specific mutations. If you have at least one F508del mutation, the most common mutation, we expect you to benefit from the CFTR modulators that are currently being developed because you are still able to make protein that modulators can correct.
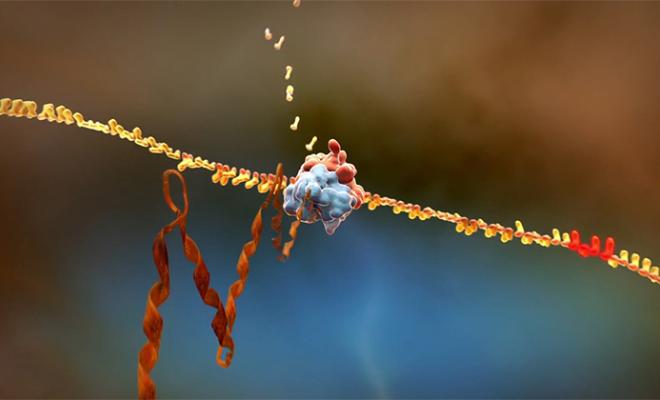
The people with CF who won't benefit solely from modulators are those who have two rare mutations that either do not produce any CFTR protein, or produce a protein that does not respond to modulators. These rare mutations include nonsense mutations (also known as “x” or “stop” mutations) in which production of the CFTR protein stops too early. This premature stop in production results in a shortened, non-functional protein that the cell recognizes as defective and destroys. Without CFTR proteins, the modulators have nothing to correct and are therefore ineffective.
Q. What potential therapies are being researched for the 5 percent of the CF population who don't produce any CFTR protein?
A. The Foundation is using a multi-pronged strategy to develop new treatments for these individuals. First, we are working with Southern Research and the University of Alabama to find and evaluate chemical compounds that “read through” or override the premature stop signal to allow a full-length protein to be made. So far, multiple molecules have shown some positive results.
Additionally, researchers at the CF Foundation Therapeutics Lab are dedicating major efforts to identify and evaluate additional readthrough compounds to determine if they could be effective therapies for nonsense mutations. The lab recently launched an initiative to create a cell culture bank with cells from people with CF who have nonsense mutations, enabling researchers to test these compounds and develop them into drugs.
In another approach, we are investing in something called ribonucleic acid (RNA) therapies. These therapies would either repair or replace defective messenger RNA (mRNA), which carries the instructions for making proteins. RNA therapy can occur in two ways: Healthy mRNA is either added directly to cells to produce a normal CFTR protein, or the defective mRNA is repaired in the cell.
RNA therapy restores the mRNA that is used as a template to create the CFTR protein in the cell, enabling the production of healthy CFTR proteins regardless of the mutation. This means that replacing or repairing the defective mRNA using RNA therapy could potentially benefit everyone with CF. We are hopeful that in the next year there will be a clinical trial to test a new RNA therapy for cystic fibrosis.
Q. What role will gene editing play?
A. The Foundation is dedicated to finding a cure for CF -- a way of restoring the defective CFTR gene -- that would benefit everyone with CF. This can be done either by replacing the entire CFTR gene (gene therapy) or repairing the defective CFTR gene inside the cells (gene editing). In order to capitalize on recent technological advances, the CF Foundation is funding research into stem cells (the cells we would target), gene editing (correcting the gene itself), and finding effective methods to deliver gene editing tools into the cells.
Although it will likely be many years before gene editing for CF will be available, it is critical that we lay the foundation now.