On July 8, I had my gallbladder removed. I had been having many problems with it and it was time for it to come out. I didn't really know what to expect. I had never gone under general anesthesia or had major surgery like it before. I went in on a Monday morning ready for my stomach issues to stop, and just a little bit nervous. I had tried not to think about the surgery until the day of because it only made things scarier for me.
The surgery went smoothly and, although there was a slight chance I could go home after the surgery, I ended up staying overnight because of a few complications. The anesthesia had caused me to vomit and the nurses wanted to keep an eye on me to make sure that I could eat and drink before sending me home.
The next morning, the nurse from the cystic fibrosis clinic came in to talk to me. She gave me lots of helpful tips that would make my recovery go a little faster. Because the surgery was abdominal, there was a good chunk of time that I could not use my vest. And for many CFers, the vest is a vital part of daily therapies. Here are a few things I did instead of using a vest after my surgery:
- I used a positive expiratory pressure (PEP) device. PEP is one of my favorite therapies. Because it was very hard for me to open my lungs and breathe deeply after surgery, the PEP allowed me to control my breathing and to focus on keeping the blue piece between the two lines for as long as I could. To get mucus out of my lungs, often I have to huff out as hard as I can. That was nearly impossible for me especially because I could barely get out of bed for the first few days. The PEP helped me maintain my breathing and didn't push me over my edge.
- Another one of my favorite therapies is an oscillating PEP device, the Aerobika®. I can now get an inhaled treatment done while working hard to get mucus out. Whoever came up with this device is a genius! It dramatically helped with my recovery too because if I got tired of doing the PEP multiple times a day, and couldn’t do harsh huff coughs, this device helped me save a little bit of time doing my hypertonic saline. It also moved a little mucus around in my lungs by forcing me to breathe in and out.
For a couple days, all I could do were those two lung therapies. But for anyone going through any kind of surgery, I have a few more tips that I believe helped my recovery. They are:
- STAY HYDRATED. I drank so much water and Gatorade that first week after my surgery that I was going to the bathroom at least a couple times an hour! My body had just gone through a super traumatic experience and needed to be replenished with liquids. Getting dehydrated after any kind of surgery can cause you to feel even more crummy. Staying on top of liquids made me feel better in the long run and helped my body get back into the groove.
- Try and move as much as you can! I know that after surgery you just want to lie down and do absolutely nothing. Trust me, I felt the same way. But I would try and get up and move at least a little bit every hour so that I could increase blood flow as well as help the healing process. And because I wasn't able to use the vest for airway clearance, getting up and moving a little bit helped with my whole body.
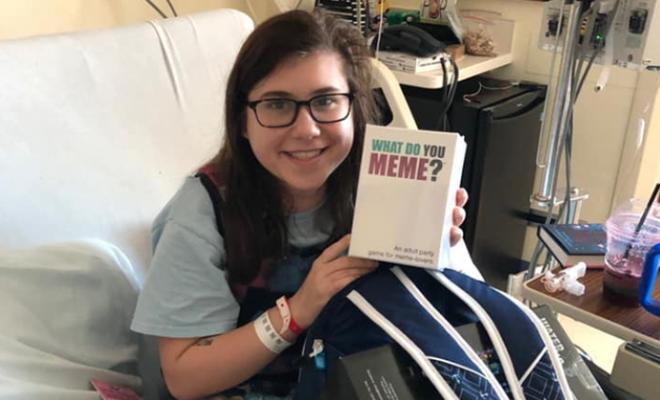
- Last, but not least, try and make the best of your surgery. It was really easy for me to get in the mindset of feeling bad and in pain, which is typical. But I tried to fill my time lying in bed with watching new shows, reading, and eating as much as I could! Surgery is never going to be an easy thing but keeping a positive mindset can help your body continue to heal as well as make your days a little less miserable. Take this time for yourself and to heal! You may never get time like this again!
Join the conversation on Facebook.