SF: What sparked your interest and focus on cystic fibrosis care? How long have you been in CF care?
PF: I had the great fortune to go to the University of North Carolina at Chapel Hill (UNC) for my pulmonary and critical care fellowship and that is where I was first exposed to CF patients and their care. It was there that I discovered my interest in CF, or should I say, that CF found me. It was the broad clinical impact, affecting so much of the body, and the very cool science that was happening at the time that drew me in. The patients and families really pulled me in, too, as they were so motivated to know about their health and how to make it better; that is what drove my enthusiasm to engage in clinical research. So, I started in 1990, and have been engaged ever since.
SF: We have a mutual connection to UNC! The gastroenterologist (GI) who diagnosed me in Savannah completed his residency at UNC and was impressed with the CF clinic there. He advised my parents to take me to UNC at eight months old for CF care because he felt they were the best; In his words, “If she were my child, I would take her there.” That was high enough praise for my parents to make the seven-hour drive from Savannah to North Carolina, and they were not disappointed. I continued my CF care at UNC until I was three years old. Even though I don't remember those days because I was too young, from the stories I've heard, it's easy to understand how one could become infatuated with the CF world at UNC. As you said, there are so many facets to CF beyond just the clinical. It's such a strong and engaging community and we, as patients, flourish when in an environment where the staff takes patient care so seriously, especially in the days prior to the internet when information was not at our fingertips as it is today.
Life with cystic fibrosis has changed dramatically over the course of your career. With that in mind, how has your practice changed because of that?
PF: The advances in science have clearly made a difference in what we use to treat patients, but my practice has evolved mostly because of what my patients and their families have taught me -- how to listen and how to communicate, and how to find out what are the most important issues, and they are not always about cystic fibrosis.
SF: That's a really interesting take. I think sometimes when you're a patient entangled in the world of chronic illness, you tend to only see improvements for your disease through the lens of science and new advances in medicine because they are tangible “things” that we can see through research and data. However, your response makes a critical point with which I agree: communication with patients and listening can be as important as medication/treatments.
What have been the most significant changes to witness in CF care, as a physician?
PF: While it is easy to focus on the newer medications and their impact, what has been most significant is the approach we, as a community, take to delivering care, and the CF Foundation has played a key role in this. The development of adult programs, transition from a pediatric life into adulthood, transparency of our data, sharing among centers, the concept of a team approach including engaging patients and families in care and research design -- these represent cultural changes in how we provide care, and they have been transformational.
SF: In the past, since there wasn't a high demand for adult CF programs, I think adults were left to manage their CF care on their own in many ways. Now, thanks to so many revolutionary discoveries, we have been able to shift thinking from ways to treat CF symptoms for a while, to actually helping people with CF plan out their lives. You are so right when you say that the programs implemented by the CF Foundation are invaluable. In addition, the internet makes these programs accessible to everyone and creates a way for CF patients to interact with each other and not feel so isolated. This shift within the CF community continues to draw us closer than ever before.
What have you found to be the most helpful element in building a rapport with patients, especially those who may be newly transitioning from pediatric to adult clinic?
PF: Spending time with them.
Time is the most valuable commodity, especially as the medical world keeps getting busier. Spending time is key to listening and learning about a person, what drives them, what holds them back.
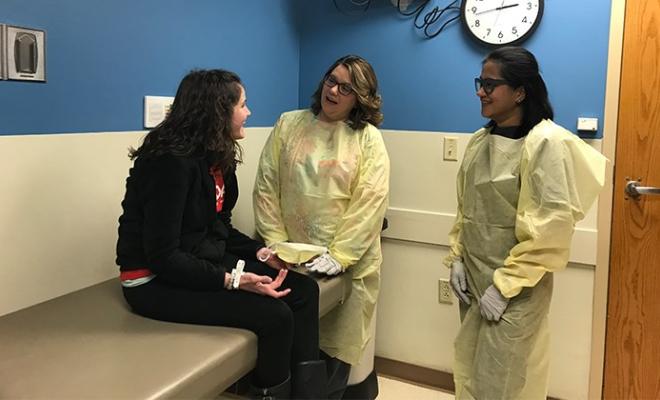
One thing I have learned from patients who have been coming to an academic program where they are exposed to trainees, getting asked the same questions over and over -- why should they share of themselves if the clinician doesn't seem to really care? So, I try to teach our young clinicians to make the time, pull up a chair and listen, engage in a conversation rather than an interrogation. Walk into the room; don't just stand at the door. Acknowledge everyone in the room. Simple stuff really.
SF: I have had many moments in my life feeling like I was being spoken “at” rather than being spoken “to,” so this really resonates with me. I remember feeling somewhat intimidated when it came time for me to transition to an adult clinic. A lot of people made it sound as though it was going to be this huge emotional cut-off. However, I have truly enjoyed attending adult clinic more than pediatric clinic because, as you said, the personnel at MUSC take time to have a conversation and make me feel like an equal. The MUSC personnel renewed my interest in my health and gave me a feeling of confidence going into appointments. I now know that no matter who I am seeing, I will be able to have a productive and engaging discussion and leave feeling like I'm ready to conquer the issues at hand. I always feel like my team has my back, which is imperative to leading a happy life with CF.
Balancing the demands of life and cystic fibrosis treatments is challenging. What is your approach to partnering with patients to help them pursue their life goals while maintaining their health?
PF: We have spent years developing tools for patients to use, but this is done with the assumption that everyone wants the same thing. I have learned from our patients that they all have different ways in which they learn and want to communicate. Some text, others email, while others will talk on the phone. So, we need to find out what works best for each person. Also, we bring so much to the clinic that it gets overwhelming; it is just too much information and perhaps the patient and their family don't leave with what we had hoped to deliver. We try to focus what happens in clinic to what we perceive is the greatest issue (with feedback from the patient, of course). But, since we still value the whole of what we bring as a team, we have increasingly tried to increase interactions using telemedicine or other approaches.
SF: I appreciate that you and your team take time to figure out what method of communication each patient will respond to best and I sincerely appreciate that they do always respond! Also, you are absolutely correct in saying that sometimes clinic can feel like information overload, especially if you're going into it not feeling well. Having alternative ways for patients to access information -- such as telemedicine or a patient portal -- is super helpful.
Many patients feel insecure about sharing information with their care team out of a fear of judgement, such as missing treatments or practices that may adversely affect their health. How does that affect the care you are able to provide and what is your approach to helping patients feel comfortable in sharing that information.
PF: I understand this very well, and since we keep tracking numbers (i.e., weight, lung function) it is hard not to feel judged. Much like the angst of taking tests in school, how do we not worry about the results and how they will be interpreted.
I tell my patients from the very start that I will never yell at them. I am greedy and want the best for them, but my goal is not to see how much therapy they can do, but to find out what works best for them. And the only way we get there is to sort it out together.
I also acknowledge that I am not the one taking the meds or doing the therapies, and I know I ask (or recommend) a lot. I have learned a lot from my patients. They teach me things that I can use with others, so sharing with me is a way to help themselves as well as others.
SF: I know from my own experiences and through chatting with other CF friends, “number anxiety” is very real and seems to be common amongst a lot of us. We all acknowledge that numbers can tell a story and it's the easiest way to see trends for a patient. However, as you said, it can be hard not to feel judged or like you've done something wrong if the numbers don't add up because we, as patients, tend to put a lot of pressure on ourselves regarding numbers. When they're up, it's exhilarating; when they're down or unchanged, it's emotionally draining. Hearing professionals give credence to our anxiety is comforting and makes the testing experience a little easier knowing that whatever the outcome is, we won't be made to feel like we've done something wrong or haven't done enough. I remember when I first started coming to MUSC how impressed and relieved I was at the fact that when somebody would come into the room they didn't immediately start talking numbers. It made the entire clinic experience a lot less taxing since I could go in knowing that whatever the outcome was, we could collaborate and figure out a plan of action.
Do you have any tips or advice for patients on how they could achieve a more open and honest relationship with their team?
PF: For a clinician to do their best, they must be up to speed with the best information, so the patient must trust their clinician. However, trust is earned. If the patient feels the clinician has not earned that trust, they need to let them know. The clinician needs to accept that this is a partnership; the clinician serves many roles (i.e., diagnostician, prescriber, coach, etc.) but cannot do it effectively if the patient doesn't share, contribute, and provide feedback.
SF: I concur. Withholding information is doing not only your team, but yourself a disservice because it makes it difficult to treat the underlying issues. However, medical settings can be daunting places and it can sometimes evoke panic when it comes time to actually talk with your doctor. That being said, as you pointed out, it does work both ways. If your doctor hasn't taken the time to make you feel like they're listening and that they see you as a person and not a number, it can create a vicious cycle of just saying anything to get out of there as soon as possible. I think clinicians and patients alike can learn that the key element of long-term care is honest communication but -- to achieve that -- you have to be willing to let your guard down a little and acknowledge that we are all just people trying to do our best.
Finally, what is the most rewarding aspect of your job?
PF: It is a privilege that I get to do this job. The mere fact that my patients trust me with this job is enough. Seeing them thrive, enjoy personal successes (school, job, travel, family) is gravy.
Interested in sharing your story? The CF Community Blog wants to hear from you.