It’s challenging to balance my physical and mental health on top of having to parent my son with his own special physical and mental health needs and be a supportive wife, beneficial therapist, and a productive business partner. Keeping up with my own treatments can be difficult. I often place my well-being at the bottom of my priority list. As a therapist, I definitely know better. It’s easier said than done, though, when there’s just so much to do.
After I had an urgent hysterectomy last year due to fibroids and endometriosis, I thought I was on my way to a life devoid of pain and illness. I was wrong. I was diagnosed at the hematologist-oncologist with essential thrombocytopenia, but my treatment team couldn’t decipher the cause of it. After extensive testing, it was discovered that I had cystic fibrosis.
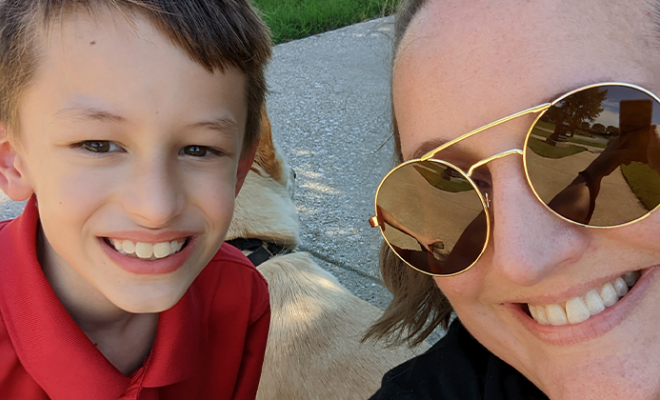
Since I’m a late-diagnosed CFer, the diagnosis came as a shock. I went through the Kubler-Ross stages of grief with anger being my favorite emotion. My son, Jesse, began going through his diagnosis of CRMS after my diagnosis, and unfortunately he was watching and paying attention. My anger at my body in turn made him angry at his body. The guilt of me being sick and passing it down to Jesse was killing me. Of course, my son also picked up on my guilt. Soon, I realized I had a problem. We had a problem. It’s hard to heal when you’re at war with your body.
Jesse and I both started seeing counselors and psychiatrists. I also got in contact with CF Peer Connect and started talking with an amazing peer. Honestly, Jesse came around to the diagnosis better than I did. He’s resilient, has a great sense of humor, and is way smarter than I’ll ever be. Of course, it helps that he has a wonderful, intelligent, and supportive father, too.
I’ve never been good at asking for help. It’s hard to ask for help when you’ve been disappointed a lot. Asking for help is hard for a lot of people, but it’s essential when you have a chronic illness.
There are times when I can’t get out of bed, or I have to stay in the hospital for a while, or I don’t have enough breath to move. Having a good support system has long been known to help improve both physical and mental health. It’s essential.
Unlike when people have other serious illnesses, such as cancer or arthritis, when we have cystic fibrosis, we can’t be around each other due to the risk of possible cross-infection. There are no in-person support groups for people with cystic fibrosis. There are in-person support groups for parents of people with CF and CRMS, but since I have CF, I’m discouraged from joining. CF is a lonely illness. Thankfully, video conferencing and social media have made it easier to communicate without the risk of cross-infection.
Thanks to CFTR modulators, like Trikafta®, many of us are living well into middle age and older. Unfortunately, Trikafta has exacerbated my depression and anxiety. I’m not alone. Plenty of others have experienced increased mood instability, brain fog, anxiety, and other neurological side effects due to Trikafta. Trikafta also caused me to have nocturnal seizures that were, thankfully, resolved with a modified dosage.
I’m new to the world of CF but I’m not new to the world of chronic illness. I’m sicker more often and for longer than I was when I was younger, such is the natural progression of cystic fibrosis. Being able to work regularly helps, and luckily, I have a job I can do from home and very supportive coworkers. Although it’s hard for many people with CF to work regularly, studies show that working prolongs life. I still try to get out in nature, walk, garden, and play outside with my family as much as I’m able. I engage in healthy coping strategies, such as meditation, yoga, Tai chi, mindfulness, journaling, expressive arts, etc. Of course, some days I don’t do any of that. My lack of energy, oxygen, and motivation gets the best of me, and that’s okay.
Interested in sharing your story? The CF Community Blog wants to hear from you.