Specialized CF Care
The benefits of seeing a care team at a CF Foundation-accredited care center is that they will recommend treatment based on CF clinical care guidelines. These guidelines are based on the latest medical evidence and best practices that make up specialized CF care so that you can receive the safest and most effective treatments.
CF Foundation clinical care guidelines recommend that people ages 6 and older visit their care center at least four times each year, receive four sputum cultures and perform at least two pulmonary function tests (PFTs) per year, as well as other annual guidelines for CF care.
During regular care center visits, your care team will monitor your health and work with you to develop and revise your treatment plan. Tests during your visit can help your team detect small changes in your health before you begin to feel badly and prevent small problems from becoming big ones.
A way to receive CF care without an in-person visit is through telehealth for those who cannot attend in person. These visits can use a range of technology, including telephone and video conference software using smartphones, tablets, or traditional computers. If you are interested in a telehealth visit, check to make sure your care center offers them and with your health insurance provider to make sure telehealth visits are covered.
The team may want to schedule shorter follow-up visits to closely monitor any emerging conditions or help you prepare for upcoming travel or transitions in your life, such as going away to college or starting a new job.
"Like many others with CF, I've recently had to adapt to telehealth appointments." — Lydia Sand, an adult with CF, from the CF Community Blog
During a Typical Visit
Care teams are made up of a multidisciplinary group of health care professionals. These professionals are trained to work together to provide specialized care. A typical visit to your CF care center may include:
Measurement of your vital signs to gauge your general health
Your nurse will measure your:
- Temperature
- Blood pressure
- Height
- Weight
Measuring your height and weight is particularly important for people with CF because it helps your care team calculate your body mass index (BMI) and determine your body composition. BMI and BMI percentile help your care team compare growth, nutrition and digestive function in people with CF to people without CF. If your BMI has gone up or down, it will help your care team understand how well your treatment plan is working.
Your nurse may also collect samples of your blood to check for things such as:
- Vitamin levels
- Indicators of liver disease
- Indicators of diabetes
- Indicators of infections
- How your body is responding to an infection
- Whether you have the right amount of certain medications in your system
- Side effects from medications
Your blood samples will be sent to a laboratory to be tested. You care team will analyze them later. The results will help your team determine if your treatment plan should change or if you should come in for a follow-up visit.
A member of your care team might share the results with you by phone or during a later visit. If your results are normal, you may not hear from your care team at all. But, if you have any questions about when your test results will come in, what your test results are or what they mean, you can always contact your care team.
https://www.instagram.com/p/BEGvBHiPxqb/
Lung (or pulmonary) function testing to measure how well your lungs work
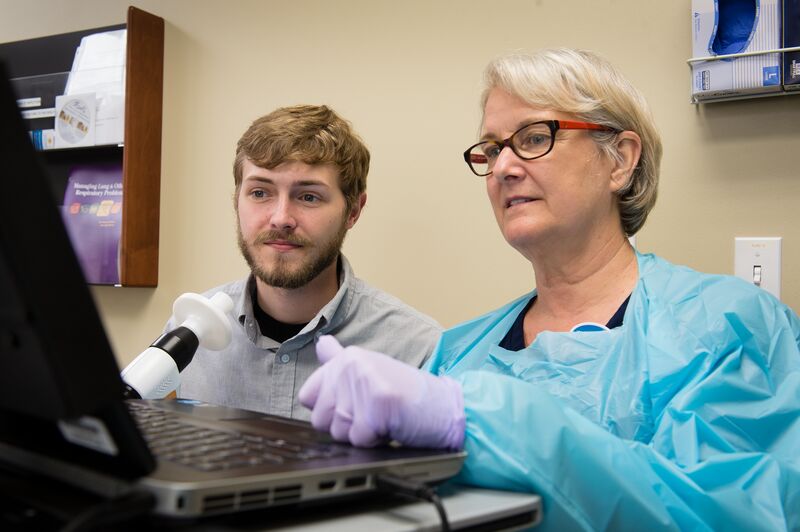
Your respiratory therapist will perform your pulmonary function test (PFT) using a machine that you blow into called a spirometer. An important result of your PFT is the FEV1 (forced expiratory volume). This measures how much air you can forcefully breathe out of your lungs in one second. This is a way to measure your lung function. FEV1 is a good measure of how much mucus is blocking your large airways.
https://www.instagram.com/p/BZymh3HhNdB/
Another important measure during PFTs, especially for children, is called the FEF 25/75% (forced expiratory flow). The FEF 25/75% is a good measure of how clear or blocked your smaller airways are. The FEF 25/75% measures the rate of airflow when you have exhaled between 25 to 75 percent of the air in your lungs.
Additional measures include how much air your lungs move in and out, how fast they move it, and how well they exchange gas (move oxygen into the blood and carbon dioxide out of the blood).
The results of your PFT during one care center visit can capture how well your lungs work at that specific point in time. But comparing that specific result to results from previous visits can help your care team see changes in your lungs over longer periods of time. Your respiratory therapist will review your PFT results with you to help you understand what they mean.
Collection of your sputum to detect and measure the presence of germs in your lungs
You will likely be asked or induced to cough during your PFTs. You will be asked to spit the mucus you cough up, also known as your sputum, into a container. Your respiratory therapist will send this sputum sample to the lab for testing. The results of the test, or throat culture, will show what kinds of germs, such as types of bacteria, are growing in your lungs. The detection of specific strains of bacteria will determine which antibiotics to use. The results are typically available in a week to 10 days.
Consultation about your diet, BMI and digestive function to determine your overall nutritional health
During your visit, your dietitian will review your diet and BMI and discuss any challenges you are facing, such as constipation or acid reflux. Your dietitian is trained to teach you how to adjust your diet so that you can get the calories and nutrients you need to meet your nutrition goals, which will help your lung function. He or she may also discuss alternative ways to get additional calories such as adjusting vitamins or digestive enzymes, adding dietary supplements or tube feeding.
Consultation about your emotional well-being and if what you're feeling is more than just the normal stress of dealing with CF
Maintaining emotional well-being is an important part of managing a chronic disease like CF. This is why your care team may talk to you about how you're feeling and offer to screen you for conditions such as depression and anxiety. These conditions, if left untreated, can interfere with your ability to effectively manage your disease and ultimately, the way you want to live your life.
Support for Affordable Care and Treatment
In addition to addressing your medical needs, you also may find help paying for your care or treatments. Your care team may include or refer you to professionals, such as a social worker or reimbursement specialist, who can work with your insurance provider or a patient assistance program to help you access affordable care or treatment options.
You also should let your care team know about changes that might affect your ability to get or pay for the health care or medications you need. Job or employment status changes can affect your health insurance coverage, which can affect where you go to receive your care or which pharmacy you can use to order your medications. If you receive Medicaid, a change in your income could also affect your eligibility.
Cystic Fibrosis Foundation Compass is a personalized service that can help you -- and your care team -- with insurance, financial, legal and other issues.
Discussing Your Treatment Plan
Your care team will review your treatment plan with you during your care center visit. This is your opportunity to discuss what is and what is not working. Although your test results are important, it is important for you to be honest and discuss how you think your treatment plan is going, any difficulties you're having fitting in your daily treatments and any changes you'd like to make.
Your care team may be experts in providing specialized CF care, but you are the expert on living with your CF. This includes:
- Knowing your body, your symptoms, and your mood -- how you normally feel -- in response to how you manage your daily treatment plan.
You can tell your care team how you feel compared to what your normal is. Your test results may not indicate an issue, such as the beginning of an infection or potential exacerbation (a worsening of symptoms), but changes you sense in your body may be important signals. If you notice that you are coughing more or feel less energetic than usual, be sure to talk to your care team about it.
- Planning ahead by talking to your care team about any current or anticipated changes in your daily schedule or lifestyle.
These changes can include short-term activities like a camping trip or international travel or more significant events in your life like, starting a new relationship, planning for a family, moving away for college, starting a new job or leaving the work force entirely.
By discussing changes in how you feel, physically or emotionally, and changes in your schedule or lifestyle, your care team may recommend adjusting your treatment plan. Ways that your treatment plan could change include trying different medications or adjusting the dose or the way you take an existing medication; trying another type of airway clearance technique; and changing your diet or your fitness routine. These changes may be temporary, or last until your health or lifestyle needs change again.